You are viewing the article Is Empty Nose Syndrome Real? And If Not, Why Are People Killing Themselves Over It? at Tnhelearning.edu.vn you can quickly access the necessary information in the table of contents of the article below.
When Brett Helling turned 36 on January 29, 2015, he was living in his parents’ basement in Worthington, Ohio, a well-heeled suburb of Columbus. His mom made him his favorite dinner: roast beef and mashed potatoes with Texas sheet cake for dessert. Brett’s friends sent him happy birthday messages on Facebook. Some asked where he’d been, why they hadn’t seen him in so long. Down the road at Natalie’s Coal-Fired Pizza and Live Music, where Brett had been working fewer and fewer bartending shifts, his co-workers texted him, begging him to come celebrate. But he didn’t want to be seen. He couldn’t do anything but lie on the couch, listless, trying to ignore the sensation of suffocation that had been plaguing him for nearly a year.
It started in middle school with allergies that only got worse over time. As an adult, Brett struggled with sinus infections that refused to go away. They clogged his ears, gave him headaches, and led to restless nights. It got so bad that in February 2014 he decided to have an ear, nose, and throat doctor perform a septoplasty, a routine sinus surgery to correct a deviated septum. His older brother had undergone the same surgery.
After lying low for about a week, Brett returned to his bartending gig. He told his doctor in follow-up appointments that something felt too “open.” The doctor assured him that barely anything was removed during the surgery, but over the next several months, Brett couldn’t shake the feeling that something was very wrong. His breathing was all messed up. In fact, he couldn’t even feel himself breathing through his nose. Instead of steady, rhythmic breathing, he felt like he was constantly coming up for air. And it was more than that. His senses felt dulled, like he’d had a lobotomy. Emotions he used to access easily now seemed far away, out of reach. Everything felt like nothing.
Brett and his girlfriend had recently moved into an old house, so at first, Carol Helling attributed her son’s symptoms to dust and other allergens. Plus, Brett could be a bit of a hypochondriac. He was always collecting vitamins and supplements to treat various ailments, and he was extremely sensitive to over-the-counter medications. He claimed he could tell the difference between Tylenol and generic acetaminophen.
Brett also tended to obsess over things, and Carol says obsessive-compulsive disorder runs in the family. As a toddler, he wouldn’t eat dinner until all the kitchen cupboard doors were closed. From high school through adulthood, he was notorious for his 45-minute-long showers; he had to wash in a certain order — neck, left shoulder, right shoulder — and if the routine got screwed up, he’d start over. He wore two or three T-shirts at a time, usually in hard-to-miss, lollipop colors.

But for most of his life, Brett’s quirks were more endearing than concerning. In fact, other than his family and some close friends, no one would have suspected he battled anxiety and depression, which surfaced most often in winter. He drank frequently, and breakups could send him into an emotional tailspin. But no one was overly concerned about Brett before his surgery. He played guitar and bass, gigging often with several bands. He was a cheerleader for his friends, especially his bandmates and others in the Columbus indie-rock community. At work, regulars would come to Natalie’s just to see him.
It wasn’t until summer that Brett’s friends and family started taking his complaints seriously. He worked fewer hours, spent more time at his parents’ house, and stopped showing up to band rehearsals. While researching his symptoms online, Brett came across something called empty nose syndrome, a rare, controversial condition that can occur after surgical procedures on cylindrical structures inside the nose called turbinates. At first, he was relieved — empty nose sounded horrific. Good thing he’d had surgery on only his septum, not his turbinates. And yet the symptoms these patients talked about sounded so much like his own. The nasal dryness. The paradoxical open-yet-suffocating feeling. Panic. Insomnia. Fatigue. Anxiety. Depression.
In August, Brett dug out his surgical report. There, alongside the septoplasty, were the two words he feared most: “turbinate reduction.” He fell to his knees, hugged his dog, and cried. He hadn’t paid attention to the other, supposedly routine procedures his doctor had glossed over. They were presented to him as fine print, as nothing to worry about.
Brett was convinced his surgery had given him empty nose syndrome, but his doctor disregarded his concerns. Another ENT physician told him he was just having anxiety. It was a conservative surgery, nothing to worry about. “Breathe through your mouth,” the doctor told him.
That fall and winter, all Brett could think or talk about was his nose. He was constantly fussing with it — rubbing it, wiping it. Co-workers who used to crave his attention began pawning him off on whomever had the time and patience to handle his obsessive rants about turbinates. By mid-October, he had checked himself into the ER and told the nurse, “I need to sleep or I’m going to die.” None of the nurses or doctors had heard of empty nose syndrome. They diagnosed him with depression, but Brett told them it was an ENT emergency. According to Brett, the ER doctor replied, “The head of ENT here doesn’t think so and will not see you.”
A few days after Brett was discharged from the ER, he began calling around to ask for painkillers and tranquilizers. Concerned friends started calling Brett’s bandmate Sean Gardner and Gardner’s wife, Mollie, who had known Brett for years and dated him in her early twenties. Mollie called Brett’s girlfriend, who told her she knew he needed help, and that she’d tried over and over again to help, but Brett wouldn’t listen to her. The Gardners decided to go see him.
“Right when we got there, we were like, ‘Oh, shit,’” Mollie says. “The dog immediately jumped into my arms. Brett’s like, ‘Sorry, he’s just looking for some normalcy. I’ve been a little crazy.’”
“He kept asking for beer,” Sean says. “We were listening to records, and he was turning them up super loud while we’re trying to talk to him. He’s pacing and kept saying the same five-minute conversation about turbinates. Over and over.”
“He wasn’t showering, not eating, not sleeping,” Mollie says. “All he could do was this loop.”
Eventually, the Gardners convinced Brett to check himself into Harding Hospital, Ohio State’s psychiatric treatment center, where Mollie works as a nurse. “He kept joking that he was kind of excited because now he would have his One Flew Over the Cuckoo’s Nest story,” Sean says.
Brett stayed at Harding about a week, and when he got out, his friends and family were hopeful. They thought he might start sleeping, and maybe the prescribed antidepressants would do the trick. But he didn’t stick with them or the psychologist. He felt like no one was listening to him. His head wasn’t the problem — someone needed to fix his nose!
In December, Brett and his girlfriend broke up. He tried to tend bar, but working while feeling on the verge of drowning was torturous. To get through a shift, he’d sometimes run to the liquor store across the street to buy a pack of gum, which helped force him to mouth-breathe. And even though music was his greatest love, he stopped playing guitar. He moved back into his childhood home, where he spent his days and nights pacing the house with Kleenex stuffed up his nose. “I can’t live like this. This is miserable,” he told his parents. “I have no life now. I want my life back. I had a good life.”
Brett was embarrassed by what he’d become. He lost all his empathy. He even envied people with cancer. Everyone has heard of cancer. Doctors take it seriously. He envied strangers blowing their snotty, functioning noses. His sinus cavity, meanwhile, felt like a hollowed-out pumpkin. In frantic attempts to explain the sensation, he’d grab his mom’s fingers and stick them up his own nose. She tried to comfort him. “Sweetie,” Carol would say. “You know we haven’t seen all the doctors there are to see. We need to do some more research. Sometimes shit happens, and we’ll get through it. It’ll be OK.”
On Monday, February 16, 2015, four days shy of the one-year anniversary of his surgery, Brett drove his green Ford Focus down Interstate 71 in the snow toward Cincinnati. After crossing the Jeremiah Morrow Bridge — the tallest in Ohio — he parked near a closed rest stop, set his iPhone on the center console, rolled down his window, and got out of the car. Snow whipped around his face. It was severely cold, the windchill well below zero. His hands were white, his cheeks red. Low temperatures dried out his nose even more than usual, and the cold air hurt. Even though his mom had recently bought him a nice orange coat, he wore only a blue hoodie, black pants, and a winter hat.
The highway was under construction, and Brett walked north along a closed portion toward the bridge. A construction worker asked him where he was going, and Brett told him he was trying to get to the other side. The worker told him that he could drive him across and that he should come warm up in his truck. Brett shook his head and kept walking. Once he hit the bridge, Brett took off running, then stopped and looked over the edge. Climbing a parapet, he dangled his legs over the side, hung on briefly, then dropped 177 feet.
Turbinate reductions are routinely performed around the world, and usually with great success. But some patients say this surgical procedure ruined their lives. In Michael Jackson’s wrongful death suit, one of his doctors testified that Jackson’s insomnia could have been a result of empty nose syndrome. Online ENS forums and Facebook support groups are filled with people who say they’ve been discarded by doctors who told them nothing is wrong — that it’s psychogenic, all in their heads. In China, one man who said he had empty nose syndrome became so enraged that he stabbed an otolaryngologist to death. Others direct violence toward themselves. When regular ENS commenters go silent online, the community wonders if they’re gone for good.
Even as some ENT doctors doubt the syndrome’s existence, a handful of otolaryngologists have made it their mission to figure out why some people develop it, how to prevent it, and whether underlying mental conditions should be considered when diagnosing and treating this invisible illness. Meanwhile, ENS patients continue to plead for help and relief.
During his ear, nose, and throat residency at the Cleveland Clinic, Dr. Steven Houser shadowed his attending physician during nasal surgeries and sometimes handled initial consultations with patients during clinic visits. One day toward the end of his residency in the late ’90s, Houser examined the chart of a middle-aged woman who was complaining of nasal blockage, congestion, and difficulty breathing. The attending doctor had operated on her turbinates years earlier. She’d had plenty of time to heal, so Houser assumed the patient must have hit her nose or maybe developed a polyp. But when he examined her, he was surprised to see that her nose wasn’t blocked at all. (“You could drive a truck through there,” Houser says.) Her septum was straight. There were no holes or other oddities, but her turbinates — those tubular, bony structures inside the nose — were significantly reduced from the surgery. The woman told Houser that for some reason, she could breathe easier when she had a cold.
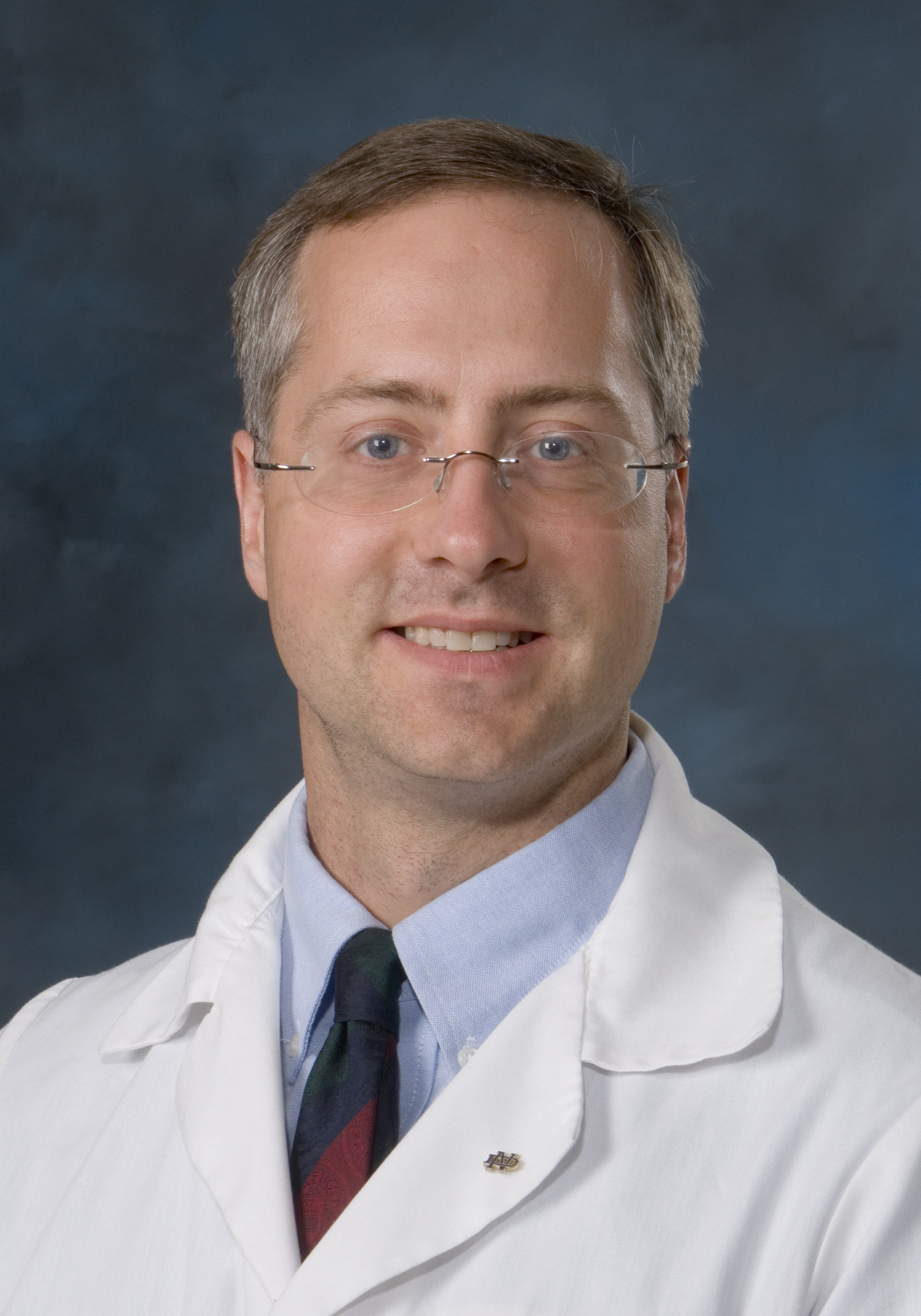
Houser was baffled. How could this woman have trouble breathing when her nose was wide open? And why would a cold make her feel less blocked? He described the situation to his attending physician, who then went into the room without Houser. After the appointment, the attending physician hemmed and hawed and never provided a good explanation. He told Houser not to worry about it.
But Houser did worry. What could explain such a bizarre condition? He did some research, and after talking to Dr. Murray Grossan, an ENT doctor in Los Angeles, he learned about empty nose syndrome, a controversial condition coined by the Mayo Clinic’s Dr. Eugene Kern in 1994. Kern described “nasal cripples” who, after turbinate surgery, suffered from symptoms like nasal dryness, crusting, and a sense of obstruction despite a wide-open nasal airway. With the help of colleagues, Kern conducted a study of 242 patients who’d been diagnosed with a rare type of nasal infection and theorized that many of these patients actually suffered from empty nose syndrome.
Not everyone in the ENT community was convinced by Kern. In a 2001 Los Angeles Times article, one physician referred to the supposed illness as “empty head syndrome.” But Houser took to the internet and began talking with people about their ENS symptoms. In one forum, he started a “Questions for Dr. Houser” thread. Some in the forum sound merely curious (“Is it good for us to swim?”). Some wonder about stem cell treatment to replace missing tissue (“Your first goal, if you want stem cells or another treatment,” Houser responds, “should be to get ENS recognized as a problem.”). Others can’t sleep and are getting desperate (“I am devastated. … I can find things to do to make it through the day; can you help me make it through the night?”). Eventually there were so many questions — nearly 30 pages of threads — that Houser’s wife was getting mad at him for spending all night on the internet. He had to stop answering questions online, but he didn’t stop his investigation.
Once patients realized an ENT doc was not only interested in their condition but also wanted to help, they began traveling from Australia, Europe, China, and the Middle East to Houser’s clinic in Cleveland. For patients Houser diagnosed with ENS, he developed an AlloDerm implant to mimic the lost turbinate tissue. Insurance didn’t cover the $9,000 to $14,000 procedure, but it seemed to be working. One of Houser’s patients self-published a book about his ENS experience: Having Nasal Surgery? Don’t You Become an Empty Nose Victim! Houser wrote the foreword.
“I’ve had about a dozen patients tell me that I’ve saved their lives and kept them from committing suicide,” says Houser, who has operated on about 70 people. “That’s why I continue to do this, because, to be honest, these patients are very difficult.”
Since Kern’s report in 2001, very little had been written about empty nose until Houser published the findings of his experimental implants in 2007, and then another article — “The Diagnosis and Management of Empty Nose Syndrome” — in The Otolaryngologic Clinics of North America in 2009. In the same journal issue, Dr. Spencer Payne at the University of Virginia published a response paper titled “Empty Nose Syndrome: What Are We Really Talking About?”
“The problem with empty nose syndrome is probably not that it does not exist,” Payne writes, “it is that we cannot adequately explain its existence by what we currently understand about the nose. Many otolaryngologists are unwilling to make a ‘leap of faith’ and, instead of acknowledging the existence of something they do not understand, are left skeptical of it in its entirety.”
While the symptoms ENS patients complain of are unique, their plight is familiar. For years, people suffering from chronic fatigue syndrome were treated with skepticism from the medical community and often told their debilitating condition was psychogenic. “Maybe these people are just lazy” was the unspoken (or sometimes spoken) refrain. BuzzFeed previously reported on a 2010 CDC study that concluded chronic fatigue patients suffered disproportionately from “maladaptive personality features” like neuroticism, paranoia, and OCD. It wasn’t until 2015 that the National Academy of Sciences pronounced chronic fatigue syndrome to be a debilitating condition with concrete physical symptoms and not a psychological illness. In the same NAS study, most patients reported it taking more than a year to get a diagnosis; a third reported it took more than five years.
Fibromyalgia patients face similar skepticism. Physicians also once believed irritable bowel syndrome was a psychological condition. Leaky gut syndrome is accepted within some corners of alternative medicine, but many doctors are skeptical of its existence. Morgellons — a more recent controversial condition involving painful, itchy lesions with mysterious “fibers” — is often regarded as a delusion, a form of psychosis.
Regardless of the validity of these contentious conditions, the experience for people who believe they have them is similar. They go from doctor to doctor, craving a diagnosis, or at least a physician who will take their complaints seriously. In one study, chronic fatigue syndrome patients said that “lack of acknowledgment could be even worse than the symptoms.” Meanwhile, the actual symptoms — which are experientially real, even if the source is debated or unknown — persist. The longer the symptoms persist, the more likely they are to either exacerbate underlying psychological conditions (anxiety, depression, OCD) or create them.
To suffer is one thing. To suffer and be told by medical professionals that nothing is wrong? That’s enough to make some people want to end it all.
Inside your nose are two bony shelves divided by your septum, and these shelves contain three sets of turbinates. Each side of the nose contains a low, middle, and high turbinate. The low one, called an inferior turbinate, is the biggest — like a small cigar, about five or six centimeters long — and inside the inferior turbinate are blood vessels that can swell and shrink dramatically. (Imagine a penis and you’re not far off.) Turbinates help regulate airflow through the nose and also warm, filter, and humidify the air using a moist outer lining of tissue called mucosa.
Allergies, sinus infections, and other conditions can cause the inferior turbinate to stay enlarged, which leads to nasal blockage. If that’s the case, and if antibiotics don’t work, it’s not unusual for an otolaryngologist to recommend reducing the inferior turbinate (and, in rare cases, the middle turbinate). There are a number of ways to do that, and there’s no consensus on which method is best. Some doctors break the bone and move the structure out of the way. Some remove about one centimeter from the head of the turbinate. Some remove the bottom third of the entire tube. Others leave the outer tube alone and remove the inside, like taking the tobacco out of a cigar. Some doctors shrink the turbinate using cauterization or radio frequency. Sometimes doctors remove the entire turbinate — a total turbinectomy — though that method has fallen out of favor in the U.S. Often these procedures are done in combination with a septoplasty to fix a deviated septum.
The CDC estimates that in 2006 (the most recent year of data), more than 900,000 people underwent nasal surgery. Though the CDC couldn’t provide data regarding turbinate surgeries specifically, the doctors I spoke to say a turbinate reduction is probably the most common procedure in rhinology, and they also say most of those patients walk away happy.
So imagine you’re an otolaryngologist operating on hundreds, maybe thousands, of patients. In follow-up appointments, almost all of them thank you for helping them to breathe normally for the first time in years. Only a handful are dissatisfied. One patient says he can’t breathe correctly. He feels like he’s suffocating. But everything looks great in his nose. The airway is completely open. The surgery did exactly what it was supposed to do.
And yet the patient keeps coming back, complaining more and more. He seems anxious, jittery, depressed. He’s not sleeping well. He’s having trouble performing everyday tasks. With each follow-up appointment, he becomes increasingly agitated. He says this routine surgery resulted in empty nose syndrome and ruined his life. You’ve heard of the condition, but you also know some doctors are skeptical of it. You certainly never spent time on the topic in medical school, where otolaryngology students concentrate on more common nasal problems, like sinusitis, deviated septum, and cancer. Not to mention the ears and throat.
Lots of other patients have appointments lined up, and they all take time. This outlier is taking time away from those patients. Eventually, you throw up your hands and discharge him from your practice.
There’s only one explanation: This patient is crazy.
Doctors like Houser in Cleveland, Payne at UVA, Jayakar Nayak at Stanford University, Subinoy Das at the U.S. Institute for Advanced Sinus Care and Research in Columbus, and researchers at Ohio State University are studying empty nose syndrome and trying to figure out why some patients get it and others don’t. Houser, Nayak, and Das treat ENS patients with implants and/or injections, and many of these patients have seen improvement. (Carol Helling says Brett received injections from Das but saw only temporary improvement; Das declined to comment for this story.)
Yet fundamental questions about ENS have yet to be answered. Are there environmental factors? Doctors in warm, humid climates like Singapore and Australia routinely perform total turbinectomies, and instances of ENS aren’t reported there as often, even though one study has shown that as many as 20% of patients who have their entire inferior turbinates removed could develop ENS.
And what accounts for the delayed diagnoses? Some patients begin experiencing symptoms months after the surgery; for others, symptoms don’t arise for years.

No one knows for sure why some turbinate reductions result in ENS and others don’t, but there are currently two prevailing theories. Houser’s theory argues that for ENS to occur, turbinate tissue must be removed or damaged, and then the sensory nerves in that area must regenerate poorly. Some methods of turbinate surgery can damage the nerve-rich mucosal layer more than others.
The other theory has to do with airflow — that the shape of a patient’s nose, and the way air flows through that nose, makes a patient more or less susceptible to ENS. Payne also thinks turbulence plays a role. “The more turbulent the airflow, the less you’re going to get a sense of good breathing,” he says. “It’s like if you stick your head out the window of a moving car, you can breathe in through your nose and feel the air moving through there, but I almost get anxious, because the air seems like it’s so poorly moving through the nose. I wouldn’t be surprised if in the empty nose patient, it’s not just a sense of decrease in receptors. It’s also an increase in the turbulence.”
The physics of airflow through the nose is complex and still not fully understood, though a study is underway at Ohio State University to better understand it. OSU’s Dr. Alex Farag and engineer/researcher Kai Zhao are developing 3D models to perform virtual nasal surgeries on patients before an actual surgery. By taking measurements and running models, they hope to see how the surgery could affect nasal airflow, which could lead to more-informed surgeries and fewer complications.
It could also be that both the airflow and mucosal/sensory theories are simultaneously true. For now, Houser and Stanford’s Nayak use cotton pledgets in the nose to help diagnose patients who complain of ENS symptoms. When the piece of cotton is inserted correctly, a patient with ENS will often feel radical improvement.
And then there’s the psychological mystery. Nayak says the ENS patients he has treated not only breathe better, they’re happier. “Anxiety, depression — all of these are off the charts for the initial patient with true empty nose syndrome,” Nayak says. He and his team are still trying to understand why that simple tubular structure seems to be essential to a proper sense of well-being for some people.
Houser can’t fully explain the relationship between mental health and ENS either. “I’ve wondered, which came first?” he says. “Were they that way, and therefore they’re more prone to nerves healing poorly after surgery and developing empty nose? Or is it the empty nose that made them so nervous and worried? I can say for sure that I’ve seen nervous, worried patients, and I implant them, and they do appear more at ease after they’re implanted. When I can get their breathing better, they’re less anxious.”
In a 2012 study in France, doctors treated a 37-year-old man with ENS symptoms who left his job and all social relationships. He spent most of his time alone in his bedroom with a humidifier. After doctors treated him with cognitive therapy and an antidepressant, many of his symptoms cleared up. “Treating ENS as a somatic symptom disorder might constitute a first-line safe alternative to surgical or even medical treatment,” the authors say.
“What we’ve seen in a lot of other chronic diseases is, each person’s perception of how bad they are is also dependent upon their general psychological health,” says UVA’s Payne. “People with poor coping mechanisms, with underlying depression or anxiety disorder — they are more likely to have symptoms that seem to take over their lives. That’s just not a normal response to chronic disease. And so you scratch your head, because as a physician, it’s the hardest thing trying to understand when are symptoms real, when are symptoms real but exacerbated by underlying psychological issues, and when are symptoms completely psychological.”
One ENS patient I spoke with, 52-year-old Sheila O’Shea, has become an informal counselor for suicidal ENS sufferers and sometimes fields late-night phone calls from them. She finds the emphasis on depression and mental health issues associated with ENS patronizing and insulting. “We’re sane people going through an insane situation,” she says. “Have you ever been stuck underwater, and you couldn’t make it to the surface fast enough? That panic you have? We have that all day long.”
She, like Brett, insists the accompanying mental condition is different from depression. “It’s as if you’re looking at the world through a big piece of Plexiglas. You can see everything and hear everything, but every experience is flat,” she says. “Depression messes with perception. Here, nothing is wrong with our perception. I’m not depressed.”
Brett Helling’s older brother, Paul, once gave him a mounted deer head he’d fished out of the trash. As a joke, Brett put the deer head in his car and drove around town with it for months. The first time Sean Gardner saw it, they were drinking beers on a Saturday afternoon in a friend’s living room. “Suddenly, this deer is banging its antlers against the window,” Sean says. “We’re all freaking out, like, ‘Oh my God!’ I run over to the side and I see Brett with this big smile. And he’s like, ‘Yeah, you just got deer-burned.’ That became his new thing.”
“He deer-burned me in the kitchen once,” Mollie Gardner says, laughing.
In the day or two following Brett’s death, Sean and Mollie wondered aloud, hopefully, if the whole ordeal was just another deer burn — the ultimate fake-out. But they knew that was wishful thinking. Once friends and family began arriving from out of town, Carol gave Sean and a few other friends one of several typed-in-advance notes Brett had left in his car near the bridge. There was also a handwritten note for the police.
“Suffering from empty nose syndrome (aka: sinus surgery gone wrong) and cannot suffocate any longer,” he’d scribbled with a Sharpie. “Please recognize this for what it really is and not just pass it off as ‘depression.’ … ENT doctors need to stop taking away perfectly good lives like mine was. This disease is very real, is untreatable, yet 100% preventable. Awareness is needed to make ENS a household name so people will stop being talked/pushed into very dangerous ‘routine’ surgery. We will continue to lose good, happy, productive, and healthy people to this disease otherwise. It took everything from me. I am not the last. www.emptynosesyndrome.org.
“P.S. Mom, I’m sorry! I held on as long as I could for you.”
The other notes went into more detail. One was a nearly 30-page script that Brett instructed Sean and three other friends to read at a memorial held at Natalie’s. The script had stage directions and specific instructions from Brett about who should read each section and even how long to pause so that certain jokes would land. It’s long-winded and rambling — angry at times (“I was ultimately killed by Empty Nose Syndrome and a salesman in a long, white jacket”) and darkly funny at others (“I felt like I was splashing around in the ocean and when Hasselhoff finally pulled up to rescue me, he just slapped some sunscreen on me and drove away on his little Jet-ski”). Brett had a way with words, but it was emotionally torturous for Sean and others to read those words on a stage in front of everyone.
“The idea of selfishly trying to end my suffering seems less and less selfish the worse things get,” Brett wrote. “I beg for your blessing in letting me go… I’m worn out, worn down and nothing feels right anymore. Our bodies are simply not equipped to deal with what I have been dealing with for so long, and I’m really sorry but I gotta get the fuck outta here, you guys.”
The memorial was so packed that Sean and others had to keep moving tables out of the way to make space for the crowd. He was thankful for the task. It gave him something to do other than sit and stare at that deer head and wonder whether his friend could have been saved.
Brett may get one of his dying wishes in 2016. Though ENS is still little-known to the general public, more ENT doctors are recognizing it and wrestling with it. In August, one of Nayak’s patients, Peter Esquinasi, wrote a letter to the American Rhinologic Society, relaying his ENS experiences and demanding a response. “Just because many people survive these types of surgeries does not mean it is the best thing for them,” he wrote. “Yours is an organization which sadly must answer this question: Do ENTs do extra surgeries for extra money? Or are they grossly misinformed? Either one is bad, but you must look in the mirror and choose one.”
The ARS executive committee responded in a letter. “We want you to know that the American Rhinologic Society is pursuing an ongoing educational effort relating to ENS,” it stated. “Your letter is of particular importance to us in the context of our educational mission.”
Dr. David Poetker, who’s on the ARS board of directors, said in an email that the ARS has no particular stance on ENS. “It is a complex issue that is not very well understood,” Poetker says. “Unfortunately, there is not a lot of money for research for nasal issues in general. We continue to do the best research we can with the limited resources available.”
In January, Dr. Das in Columbus noted a sea change in an open letter to ENS patients he posted on the emptynosesyndrome.org forum. ENS, he said, is the thing keeping some of his colleagues up at night. “There continues to be greater recognition that ENS is a problem,” Das writes. “Many panels within the American Rhinologic Society are discussing ENS as a real problem and leading discussions on the best way to solve this problem.” Das’s letter also expresses hope about the injection therapies he’s tried on 180 patients from 25 countries; 82% of them reported an improvement in their symptoms.
And it’s no small thing that a press release for Ohio State’s nasal surgery study mentions empty nose syndrome by name, even though Carol Helling says Ohio State doctors told Brett he didn’t have it.
In some ways, Brett’s case was typical. His symptoms overlapped with many others who say they have ENS. The problem is, there’s still no firm definition of empty nose syndrome, which means there’s also no firm way of diagnosing it. And misdiagnosis is an issue. Houser and Nayak say they’ve seen patients who were convinced they had ENS but had a different nasal problem entirely.
“My research group is trying to lay the groundwork for better defining ENS, and pulling it out of the ‘mysterious, not sure it exists’ bucket, into the ‘definite diagnosis with defined parameters’ category,” Nayak says. Recently, Nayak and his Stanford researchers analyzed CT scans of patients diagnosed with ENS and compared them to patients who underwent turbinate reduction surgery but had no ENS symptoms — a comparison that had never been done before. “We detected a statistically significant central location in the nasal airway that swells in the CT scans of ENS patients, but not in any control patients,” Nayak says of the soon-to-be-published study. Nayak’s group also came up with six questions he says will more accurately diagnose ENS. He and his team will present their findings at a national meeting of otolaryngologists in Chicago in May.
Doctors’ responses to the presentations could determine how ENT doctors approach ENS moving forward. Will Nayak’s research — along with the work from Ohio State, Das, Houser, and others — finally put the skepticism to rest, or will doubt persist? If the data resonate, will doctors alter their surgical methods? And will those changes spill over to the cosmetic surgery community, where doctors performing nose jobs are probably even less familiar with ENS?
Turbinate reductions aren’t likely to go away, despite outcries of malpractice from ENS patients. Every otolaryngologist I spoke to, including those who acknowledge the dangers of ENS, continues to perform surgeries on turbinates. A friend of Brett’s recently wrote to his congressman to propose a bill that would require doctors to warn patients about the risks of ENS before turbinate surgeries, but even Houser says that goes too far. “The rate of ENS development is so small, and if turbinates are treated properly, ENS should essentially never occur,” Houser says. “The focus should be on educating doctors of proper techniques.”
Houser also often requires patients to undergo mental health assessments before he considers surgery, and Payne says he’s similarly vigilant. “There are some people I’ve refused to do surgery because they were people who I felt were setups for an empty nose scenario,” Payne says.
In January, Brett Helling’s friends celebrated his life with a two-day concert dubbed “Helling Yeah!” at Natalie’s. (The promotional poster featured a giant deer head.) At first, the organizers wanted proceeds from the event to benefit ENS awareness, as well as suicide prevention. But there’s no vetted, surefire way to contribute to ENS awareness yet. Despite the strides in research, it’s still nebulous, still opaque.
Just a couple of weeks before the benefit concert, a frightened new visitor to the Empty Nose Syndrome Facebook page posted a desperate plea.
“Please help! I had surgery December 7, 2015,” she wrote. “I feel the nasal passages as huge tunnels, the cold air burns the nose and throat. … I’m going crazy, no sleep 8 days. What do I do? I don’t want to die.” •
Thank you for reading this post Is Empty Nose Syndrome Real? And If Not, Why Are People Killing Themselves Over It? at Tnhelearning.edu.vn You can comment, see more related articles below and hope to help you with interesting information.
Related Search:

